45+ Free Therapy Progress Notes Templates
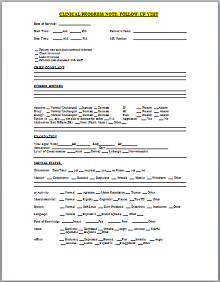
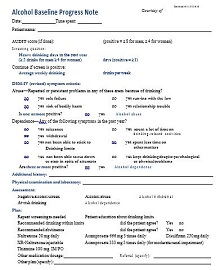
A medical progress note template is a report that describes the medical history of a patient. Progress note describes the health status summary of a patient that is used to inform healthcare professionals about the medical history, treatment plans, prescribed drugs, and other important information.
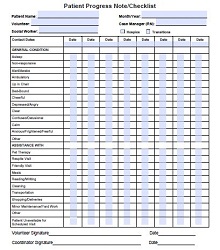
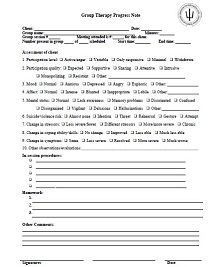
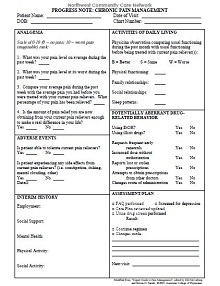
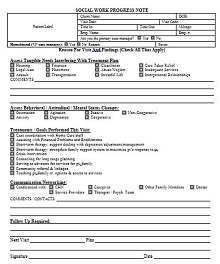
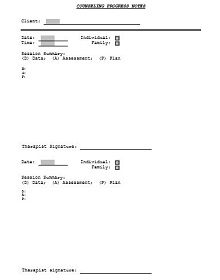
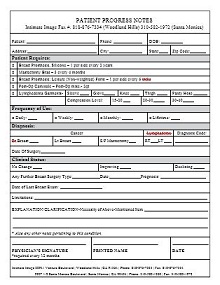
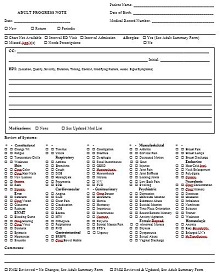
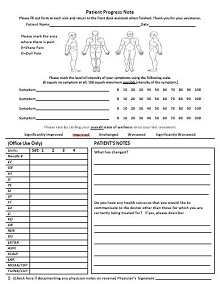
A therapy progress note is one of the most important documents to follow up on the treatment of a patient. Progress note templates provide an outline to create it effectively using SOAP or PAIP format. The medical progress notes are created by the doctor, nurse, and other health care workers. The sample patient progress notes help you to get started. You can find here patient progress notes samples and templates for physicians, therapists, dentists, and consultants in PDF and DOC formats to maintain the record of patients in a better way. In this article, you can find everything about patient progress notes.
- Accounting Templates
- Art & Media
- Budget Templates
- Business Templates
- Calendar Templates
- Certificates
- Charts
- Education Templates
- Inventory Templates
- Invoice Templates
- Letter Templates
- Medical Templates
- Personal Templates
- Project Plan Templates
- Timesheet Templates
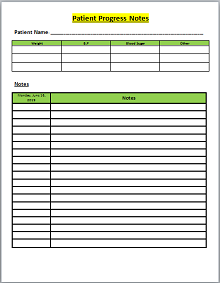
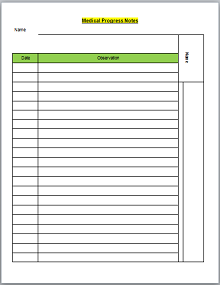
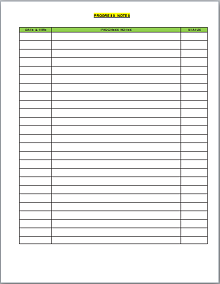
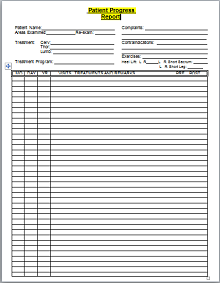
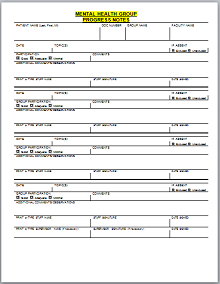
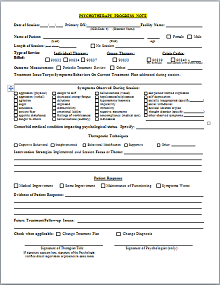
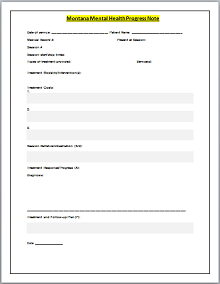
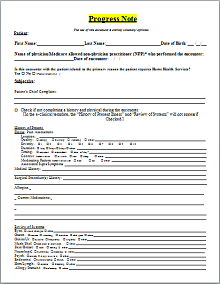
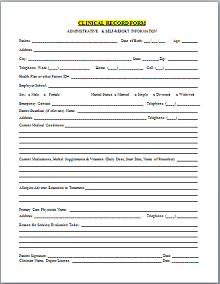
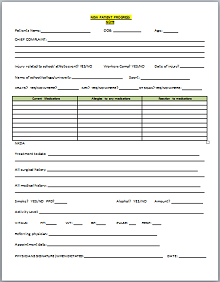
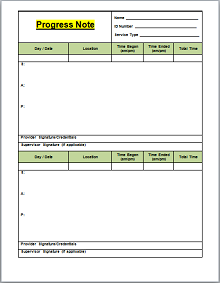
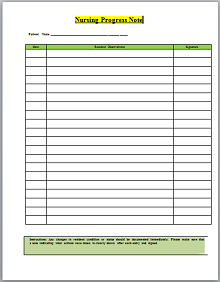
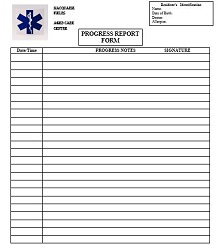
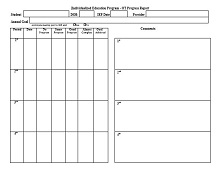
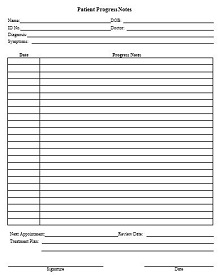
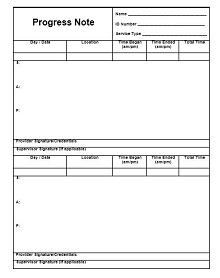
Download Free Progress Notes Templates
A Progress note is created and used by healthcare professionals. Documenting the medical record or history helps in monitoring the progress of a patient.
A progress note template usually has four parts :
- Subjective: It describes the patient’s conditions like pain, reaction, etc.
- Objective: This part describes the results of the laboratory test.
- Assessment: It contains information about the disease which is diagnosed by a doctor.
- Plan: Details about the treatment chosen by a healthcare professional.
Here you will find a complete list of progress note templates.
What is a Progress Note?
A progress note is one of the most important documents to know the patient’s current status, diagnosis information, and achievement during the patient’s treatment. The patient’s progress note is a vital component of the patient’s medical history when different healthcare workers participate in the treatment of patients. It is created and used by doctors and nurses to communicate the patient’s condition effectively. If a patient is not satisfied with the treatment and wants to consult a new doctor, then a progress note is an essential document for the new doctor to provide better treatment. It is also useful when a doctor is off duty, and a new doctor handles your course of treatment.
The life of a doctor is so busy they eliminate all the unnecessary things from their life. We make their life easier by providing ready-made templates of progress notes; you can also see our fantastic collection of doctor’s prescription pads and doctor’s note templates that make your work easier. It would be better if the doctor and nurse’s notes were taken hourly for better monitoring of the patient.
This medical progress note should be written clearly and must include all the essential information that adequately describes the condition of the patient. If you write the progress note using a standard format like PAIP and SOAP, then it is more understandable, informative, and brief to define all the things clearly. Most healthcare care professionals use the SOAP method to write progress notes. If you want to improve the documentation of your progress notes, then you should see the progress note example and download templates to create it effectively.
Importance of Progress Notes
A progress note is an essential document in the medical record of a patient. It is used to get the response of a patient during treatment. Below we share some points that help you to know the importance of it.
- During medical treatment, it is essential to know the patient’s medical condition under this treatment; progress notes help you to compare the patient’s status at different stages.
- It is important when different healthcare workers provide the therapy at different times, just like when the nurse shift changes, then the new nurse reads the patient’s progress note and takes care of him according to it.
- It is the best way to monitor the patient’s progress to know whether the condition of the patient is good, bad, or the same.
- It works as a record of a patient’s illness, diagnosis information, and course of treatment.
- If you go to the new doctor for treatment, then he/she will not start your course of treatment until the doctor knows the patient’s medical history or progress note.
- With the help of progress notes, doctors provide better courses of treatment for the patient.
- Healthcare providers judge patients’ behavior and plan or change the line of treatment based on it.
- If you have medical insurance, then this document is useful to submit a claim for the reimbursement of medical expenses to the insurance company.
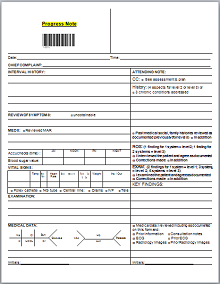
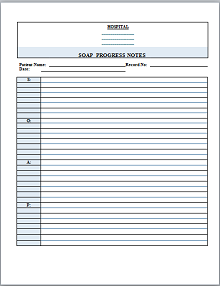
What are the SOAP Progress Notes?
Documenting the progress of a patient’s condition is a crucial task. It should be written clearly to know the patient’s status. While writing progress notes, most healthcare providers use the SOAP method to make this document informative, comprehensive, and detailed. It is the most widely used format by doctors, nurses, and other health care providers to write the patient’s progress in a specific order.
The components of the SOAP provide the details of the patient’s situation, what the nurse or doctor observes, diagnosis details, and the course of the treatment. Most doctors, therapists, consultants, and dentists use the SOAP format to write progress notes. SOAP is a standard format for writing progress notes to make it understandable to everyone. A SOAP progress note has four components: subjective, objective assessment, and plan. Sections of SOAP notes are as follows:
- Subjective: It is the first section of progress notes which contains information about the patient’s expression. The information verbally provided by the patient is written in this section. For example, the patient complained of pain in the left arm.
- Objective: The objective section of progress notes contains the observations that nurses or doctors measure, see, and feel. It includes the details of the symptoms that you feel, such as temperature and pulse. It also contains lab tests such as X-rays and blood test reports.
- Assessment: The assessment section of SOAP progress notes contains the diagnosis details. In some cases, it may not be a definitive diagnosis. The assessment section is written based on objective and subjective sections. It contains the analysis, and diagnosis details, and indicates the goals and the progress of the patient.
- Plan: This step of the SOAP progress notes provides the outline of the course of the patient’s treatment. It contains information about how to handle the problem of the patient, medication, treatment, and details of the next steps for the other healthcare provider.
In our collection, you can find the blank SOAP progress notes samples and templates in PDF and DOC formats that make your work easier and help to write it effectively.
Things to Include in the Progress Note
A progress note is an important document in the medical record of a patient. Progress notes should be written in a way that is easily understandable by other healthcare providers. It should include all the necessary things that make it effective and useful for every purpose. Things that should be included in the doctor’s progress note are as follows:
- Patient’s information: The patient’s name, address, phone number, gender, age, and relationship status must be included in it.
- Clinic information: The name of the clinic with its address, phone number, logo, and other necessary information should be included in it.
- Patient’s complaint: It should include the patient’s complaint that he/she describes verbally. It’s very helpful to judge the medical condition of the patient.
- Symptoms: Symptoms nurses or doctors observe that the patient has.
- Medical history: It contains information about allergies, medication history, and previous diseases that describe a person’s past medical issues.
- Medication: Details of medicine that the doctor prescribed.
- Treatment: It should include information about medical treatment or procedures that healthcare workers provide.
- Discharge details: At the end of the progress notes, it should contain the summary of discharge.
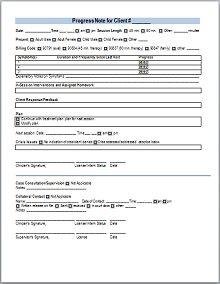
The above things are essential and must be included in the patient progress notes. A psychotherapist progress report is used to record the content of the conversation with the patient during a session. You can download psychotherapy progress note samples and templates to assess the problem of the patient efficiently. Most healthcare providers use SOAP or PAIP format to write daily progress notes. It is always easy to work with templates; you can get printable progress note templates that help you make a comprehensive report of a patient’s medical condition.
How to write the Progress note using SOAP?
SOAP is the most popular and widely used method to write compelling and useful progress notes. Usually, healthcare providers create a progress notes checklist to complete it quickly and efficiently. The SOAP progress notes template is written by healthcare professionals to provide detailed information about a patient’s health and course of treatment. Below we share a few steps that help you write the SOAP progress notes:
- Step 1: Download the SOAP progress notes in the format that you prefer.
- Step 2: Start with the patient’s name and other essential information.
- Step 3: Write down the goal list of the patient.
- Step 4: S–Subjective: Gather all the information that the patient tells you about the medical condition and write it in the subjective section of the progress note. The OLD CHART acronyms are the best way to quickly and efficiently write all the patient concerns.
- Step 5: O–Objective: Write down the detailed observation about the patient’s expression and body language. Write about the lab reports of the patient, such as x-rays and blood reports.
- Step 6: A–Assessment: The assessment section of the progress note is based on the objective and subjective parts. State the diagnosis details, treatment procedure, and condition of the patient, whether it is worse, excellent, or the same.
- Step 7: P–Plan: In this section of progress notes, write about the course of the future treatment, therapies, tests, medication prescribed by the doctor, and next visit date.
- Step 8: Discharge details: At the end of the progress note, write the date when he/she is discharged from the hospital with a quick short review of the initial state of the patient, symptoms, tests, treatment, and other necessary information.
Tips for Writing the Progress Notes
Below we share some tips that help you to write a useful progress note for mental health, dental, therapy, and all other medical problems.
- Use a standard format: If you want to write a progress note that is informative, brief, and easily understandable by everyone, then you should use a proper format such as SOAP or PAIP to write it effectively. When you use a standard format to write a paper, it allows other healthcare providers to understand what steps you’ve taken to solve the patient’s problem.
- Should be legible: You should write the progress notes in a manner that increases their readability and is quickly understood by every person. Don’t use wordy sentences, poor grammar, and passive voice sentences in your document. It should be written clearly and concisely.
- State the medication and treatment clearly: Make sure the medication prescribed by the doctor and the treatment or procedure should be clearly defined. It helps the healthcare worker to provide better treatment in the future.
- Take notes each hour: It would be best to take notes each hour when the patient’s condition is critical. You can take progress notes after 2 or 3 hours when the patient’s condition is not critical. For the patient’s care, it is necessary to write your observation every hour.
- Write related information: The things included in the progress notes should be related to the medical problem and treatment. Don’t write irrelevant stuff in the patient’s progress notes that create confusion.
Benefits of SOAP Progress Notes
In medical progress notes, SOAP is widely used to write it. It is a useful way to clearly state all the things regarding a patient’s health. Some significant benefits of SOAP progress notes are as follows:
- Keep your record clean: In health care professionals, there are different ways to monitor the progress of a patient, but the SOAP progress note is one of the best ways to track the patient’s illness and treatment efficiently. Progress notes are an important part of medical history that may be helpful for better treatment in the future. The SOAP format keeps your record clear, concise, complete, and accurate.
- Enhance the quality of documentation: The SOAP framework enhances the readability of the document which helps to maintain the patient’s progress note efficiently. The four parts of it allow the reader to understand all things clearly.
- Best communication tool: It is the best way to communicate with the patient clearly and concisely. It allows other healthcare providers to communicate for the better treatment of patients. If a patient visits a new doctor, this progress note helps the other healthcare worker understand the patient’s condition quickly and easily.
- Accuracy and efficiency: When doctors use different frameworks to write notes, it isn’t easy to understand each one. It is a standard format of writing progress that helps the healthcare provider to get on the same page. This method increases the accuracy and efficiency of the document, creating less confusion, and achieving the patient’s end goals.
Frequently Asked Questions
What does PAIP stand for?
The problem, Assessment, Intervention, and Plan(PAIP) is the method of writing progress notes by healthcare providers.
Difference between Psychotherapy notes and progress notes?
The mental health professional writes psychotherapy notes during the session with a patient, whereas a progress note is used to monitor the patient’s illness and course of treatment.
What are the four components of SOAP?
The four components of SOAP are Subjective, Objective, Assessment, and Plan.
Why do we write progress notes?
A progress note is used to track the progress of a patient’s health. It is a way to communicate with other healthcare providers and inform them about the course of treatment you’ve taken to solve a problem.
Is a SOAP note a progress note?
SOAP is a method to write progress notes. A progress note written by using the SOAP format is called the SOAP progress note.
How often should progress notes be taken?
It depends on the patient’s medical condition; if the patient’s medical condition is critical, then progress notes should be taken in each hour; otherwise, it should take after 2 to 3 hours.