45+ Free Medical Soap Note Example & Format – PDF
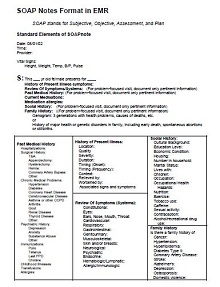
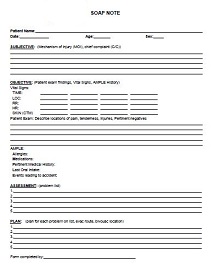
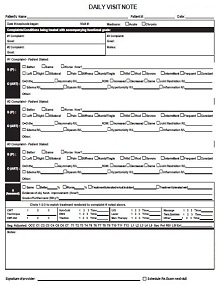
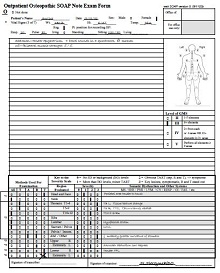
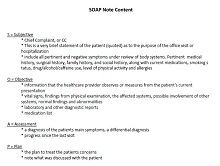
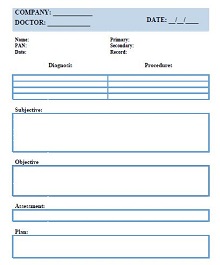
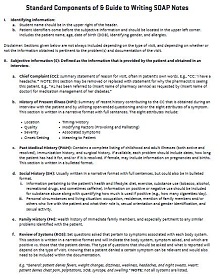
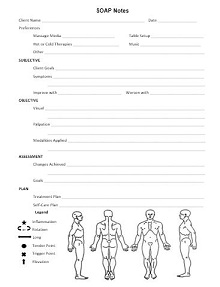
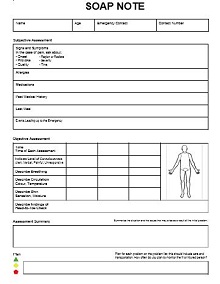
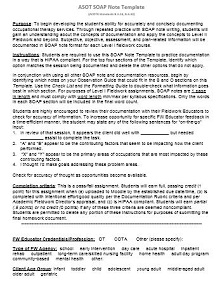
A soap note(subjective, objective, assessment, and plan note) is a progress report used by healthcare providers to document the details of a patient encounter. These notes consist of four main sections subjective information, objective observations, assessments, and plans for follow-up care. The subjective section includes the patient’s description of their symptoms and any additional health information they may provide.
The objective observations are those the provider can observe during an examination or diagnostic testing. Assessments detail any diagnoses that have been made based on findings discussed in the prior two sections and finally, the plans for follow-up care explain what treatments should be provided going forward. Health professionals rely heavily on these notes to keep track of what has been going on with a patient’s medical condition and to plan treatment moving forward.
- Accounting Templates
- Art & Media
- Budget Templates
- Business Templates
- Calendar Templates
- Certificates
- Charts
- Education Templates
- Inventory Templates
- Invoice Templates
- Letter Templates
- Medical Templates
- Personal Templates
- Project Plan Templates
- Timesheet Templates
Download Free Medical Soap Note Example & Format
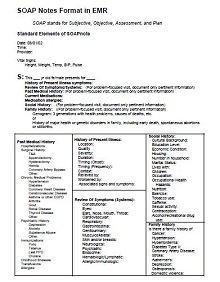
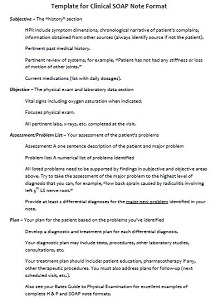
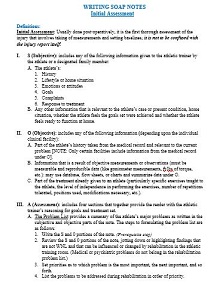
What are SOAP Notes?
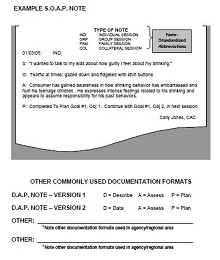
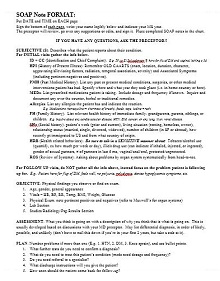
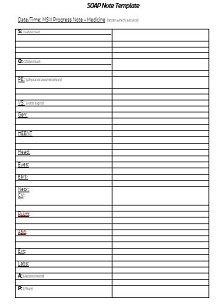
SOAP notes are an organized method of documenting information in a patient’s medical chart. Typically used by healthcare professionals while providing medical care, SOAP stands for Subjective, Objective, Assessment, and Plan. The subjective part reflects what the patient is reporting, their history, current symptoms, and so on. The objective component involves facts uncovered in the physical examination and lab tests.
The assessment segment contains the professional’s interpretation of the data gathered and impressions of the patient’s condition. Lastly, the plan outlines any additional steps that need to be taken to properly treat the patient such as referrals to specialists or medication changes. Together these four categories make up a convenient format for recording a complete understanding of a patient’s current condition as well as a game plan going forward to help ensure they receive quality medical care.
Why Are SOAP Notes Important?
The importance of SOAP notes lies in providing an organized system for documentation that can be easily accessed and understood by other healthcare professionals. This is especially important when dealing with complex cases or managing multiple patients at once.
By using SOAP notes healthcare providers can quickly review a patient’s history without having to go through long documents or decipher messy handwriting. Additionally, having a clear record of interactions makes it easier to track progress over time and identify potential problems before they become worse.
Benefits of Using SOAP Notes
There are many benefits to using SOAP notes in your practice. Here are just a few of them:
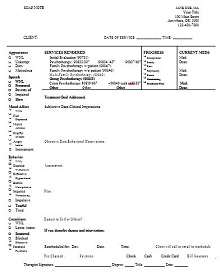
- Improved communication between clinicians – When all members of a healthcare team have access to a patient’s SOAP notes, it makes it easier for everyone involved to keep up with the details of their care plan. This helps ensure that everyone is on the same page about what needs to be done for each patient.
- Easier documentation – When you use SOAP notes, you don’t have to worry about writing detailed reports or long summaries after each visit with a patient. Instead, you can simply fill out the brief form which makes documentation much easier and more efficient.
- Improved accuracy – Because they are structured documents, SOAP notes help reduce errors in documentation by providing clear guidelines on what should be included in each field. This helps ensure that all relevant information is accurately recorded so that clinicians can make informed decisions when providing care for their patients.
How to Create a Soap Note Sample Effectively
A soap note sample is an effective way to document a patient’s progress over time. This format provides healthcare professionals with the necessary information to provide better care and ensure that each patient gets the best treatment possible. Here are some steps on how to create a soap note example effectively.
Getting Started
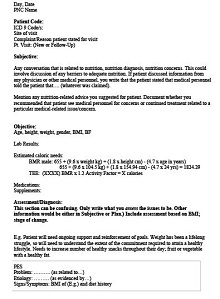
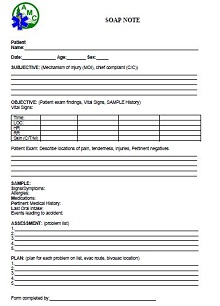
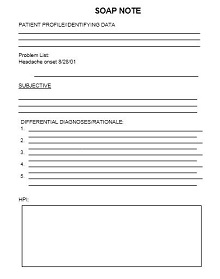
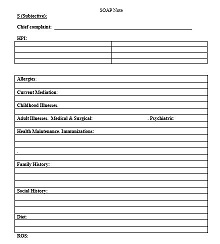
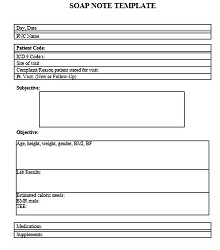
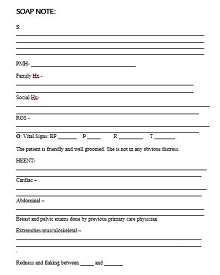
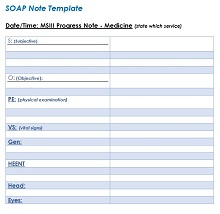
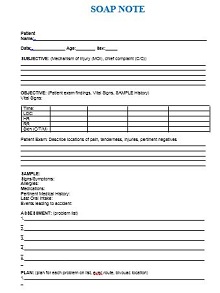
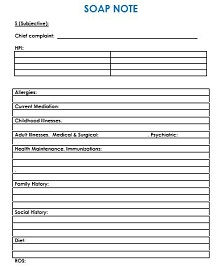
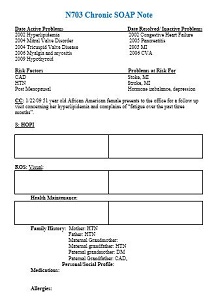
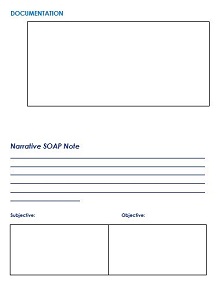
The first step in creating a SOAP Note Template is to gather all of the necessary information about the patient. You’ll want to include their medical history, current medications, symptoms, lab results, and any other relevant data. Once you’ve collected all of this information, you can begin organizing it into the four sections of the SOAP Note Subjective, Objective, Assessment, and Plan.
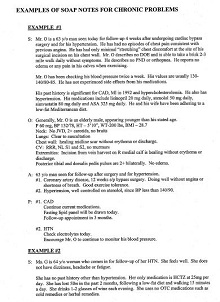
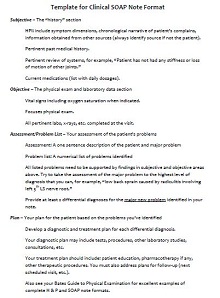
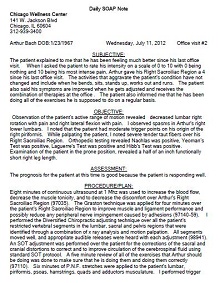
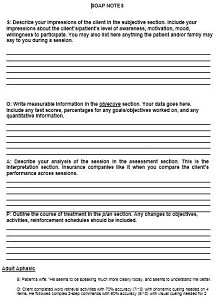
Subjective Section
In the Subjective section of your note sample, you will detail the patient’s own description of their health and symptoms. This includes things like pain levels or any changes in behavior that they have noticed since their last visit. Be sure to record this information accurately so that it can be used as evidence when evaluating the patient’s overall health status.
Objective Section
The Objective section is where you will record your own observations of the patient during their visit or treatment session. This can include things like vital signs (temperature, heart rate, respiration rate) physical exam findings pulse oximetry readings, or laboratory test results (CBCs). It is important to be as detailed as possible so that you are able to accurately identify any changes or trends over time.
Assessment Section
In the Assessment section of your note sample, you will explain what you believe is causing the patient’s symptoms or condition as well as how it can be treated or managed. This should also contain any diagnostic tests that were done and what their results were as well as any follow-up appointments that need to be made in order to monitor progress or further assess any changes in condition over time. Be sure to include references from medical literature if applicable so that others reading your notes can get a better understanding of why certain decisions were made regarding treatment plans for each individual case.
Plan Section
Finally, in the Plan section of your note sample, you will outline what steps need to be taken in order for the patient’s condition or symptoms to improve or resolve completely. This should include both short-term goals as well as long-term goals depending on how severe each individual case may be. Additionally, if there are lifestyle changes that need to occur in order for improvement or resolution such as diet modification or exercise guidance then those should also be included here along with specific recommendations if applicable such as dietary supplements or prescription medications needed for symptom management/resolution purposes if necessary. Ensure that all aspects have been thoroughly discussed including potential risks associated with certain treatments before finalizing your SOAP Note Example.